Listeria
History & Epidemiology
In 1911, G. Hülphers described bacteria that he isolated from the diseased liver of a rabbit. Hülphers named the bacteria Bacillus hepatis, and his description closely matched the findings of E.G.D. Murray 15 years later. In 1926, Murray isolated bacteria from the livers of sick rabbits and guinea pigs and named the bacteria Bacterium monocytogenes. The bacteria went through several more name changes, and in 1940, the name was officially changed to Listeria monocytogenes to honor Joseph Lister, the British surgeon who discovered that sterilizing surgical instruments before operations reduced the risk of infections.
In 1929, A. Nyfeldt reported the first confirmed cases of listeriosis in people. But L. monocytogenes weren’t identified as a major cause of foodborne illness in people until the 1980s when several large outbreaks occurred. Since the 1980s, there have been about 80 recognized outbreaks of listeriosis in people.1
Compared to other foodborne illnesses, listeriosis is rare but very serious. Even with adequate antibiotic treatment, the disease has a high mortality rate of 20 to 30 percent.Over 90 percent of people with listeriosis are Hospitalised, often in intensive care units.
The World Health Organization estimated that worldwide in 2010, listeriosis sickened 23,150 people, and of these, 5,463 died.
L. monocytogenes is widespread in the environment, especially in soil and water. The bacteria can survive in soil for many months. Animals, particularly cattle, can carry L. monocytogenes without appearing sick and shed the bacteria in their feces.
The bacteria are able to live in a wide range of conditions and environments—they can tolerate both acidic and salty conditions, both high and low temperatures, and a fairly low moisture content. These characteristics allow L. monocytogenes to survive a long time in a variety of food products and food processing plants. Because the bacteria can multiply and persist in food processing plants for years L. monocytogenes is especially hard to control and can result in intermittent contamination of food. Unlike most bacteria, L. monocytogenes can grow and multiply at low temperatures, making the bacteria a potential problem even in properly refrigerated food.
how people can become contamined
People become infected with L. monocytogenes by eating contaminated food. People can also become infected by handling contaminated food, such as contaminated pet food, or touching contaminated surfaces and utensils and then accidentally transferring the bacteria from their hands to their mouths. Babies can become infected in utero or at birth if their mothers ate contaminated food during pregnancy.
The bacteria can contaminate a variety of food, such as:
Raw meat
Ready-to-eat processed meat such as hot dogs and deli meat (both factory-sealed packages and products sold at deli counters)
Raw vegetables
Refrigerated pates
Ready-to-eat smoked seafood and raw seafood
Prepared or stored salads, including coleslaw and fresh fruit salad
Melons
Soft cheeses made with unpasteurized milk
Unpasteurized milk and milk products.
Pasteurization, cooking, and most disinfecting agents kill L. monocytogenes. However, in some ready-to-eat food, such as hot dogs and deli meats, contamination may occur after the food is cooked in the factory but before it’s packaged. These products can be safely eaten if reheated until steaming hot.
listeriosis in people
Listeriosis occurs almost exclusively in pregnant women, newborns, the elderly, and people with weakened immune systems (such as those with cancer or other diseases). After a person ingests L. monocytogenes, the bacteria grow quickly in the liver and then move into the bloodstream and can invade many places in the body, including the:
Brain
Membranes surrounding the brain and spinal cord (called the “meninges”)
Gastrointestinal, or digestive, tract (the stomach and intestines)
Liver
Bloodstream.
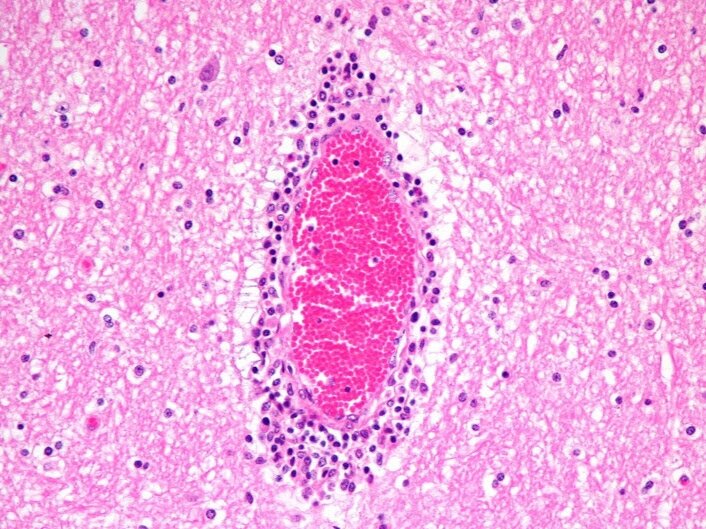
Liver: Acute - subacute hepatitis with necrosis
Brain: perivascular cuffing lymphoplasmacytic
Spleen: white pulp, granulomatous
Pregnant Women and Newborns
Pregnant women are 18 times more likely to get listeriosis than other healthy adults, and 16 to 27% of all L. monocytogenes infections are in pregnant women.Scientists don’t know why pregnant women are so susceptible to the disease. It usually affects pregnant women who are healthy and don’t have other risk factors.
Diagnosing listeriosis in pregnant women is difficult because they usually don’t have the gastrointestinal symptoms—such as vomiting and diarrhea—that are normally seen with a foodborne illness. The most common, and sometimes only, symptom of listeriosis in pregnant women is fever. They often have a flu-like illness with non-specific symptoms, such as fatigue and muscle aches, which are often temporary and go away on their own. Some pregnant women show no symptoms. In a series of 191 cases of listeriosis in pregnancy, over one-quarter (29%) of the women had no symptoms.
While listeriosis in the mother is mild, infection in the fetus and newborn can be severe. Listeriosis can develop at any time during pregnancy, and the disease causes miscarriage, stillbirth, premature birth, and life-threatening infection of the newborn, such as a blood infection, respiratory distress or pneumonia, and meningitis (inflammation of the membranes surrounding the brain and spinal cord). Listeriosis is one of the most common causes of meningitis in newborns. With a mortality rate of 20 to 30%, newborns suffer the most serious consequences of listeriosis. They have either early- or late-onset disease depending on when their symptoms first appear.
non pregnant people
Healthy children and adults occasionally get listeriosis, but rarely become seriously ill. In healthy, non-pregnant people, listeriosis can cause gastroenteritis—mainly diarrhea—accompanied by a fever. Other symptoms may include vomiting, joint pain, headache, and body pain. This form of listeriosis has a much shorter incubation period, with symptoms typically occurring within 24 hours after a person ingests a high number of the bacteria. The illness is usually mild and goes away on its own. The diarrhea can last up to 5 days
The elderly and people with weakened immune systems have a higher risk of getting a more severe form of listeriosis, including:
Inflammation of the brain (encephalitis)
Inflammation of the membranes surrounding the brain and spinal cord (meningitis); and
Infection of the blood.
preventing listeria infections
There are three very simple things you can do to help prevent illness from Listeria:
1. Chill at the Right Temperature
The right temperatures slow the growth of Listeria. Put a refrigerator thermometer in the refrigerator and adjust the refrigerator temperature control, if necessary. Put a second thermometer in the freezer. Your refrigerator should register at 40°F (4°C) or below and your freezer at 0°F (-18°C).
2. Use Ready-to-Eat Foods Quickly!
Use ready-to-eat, refrigerated foods by the Use By date on the package. The longer they’re stored in the refrigerator, the more chance Listeria has to grow.
3. Keep the Refrigerator Clean
Clean your refrigerator regularly. Wipe up spills immediately. This is particularly important, so Listeria doesn’t have a place to grow and then spread to other foods. Clean the inside walls and shelves with hot water and a mild liquid dishwashing detergent, rinse, then dry with a clean cloth or paper towel.